UK Labour Government opens up the National Health Service to further privatisation
Introduction
The NHS in the United Kingdom was set up following the Second World War. Perhaps one of the best achievements of the ‘old’ Labour Party it was a major reform. It followed the realisation by the British ruling class that:
i) The USSR in 1945 exerted a huge influence on British workers;
ii) the working class of Britain was not healthy enough to either create the most profit for the ruling class; or to be the best recruits for the armed forces.
Nevertheless it did provide excellent health services for the people of Britain free at the point of access. By any parameters it helped to ensure a healthy population.
Since the austerity regimes of Margaret Thatcher for the Conservative Party, and the Labour Party under Tony Blair – this was steadily eroded. Now under the current Labour leadership of Sir Keir Starmer, the doors are held open for private finance even more firmly. His Secretary of State for Health – Wes Streeting – has a long track record of having helped Starmer to purge the Labour Party of traditional leftists. His philosophy comes out clearly in his stated view that he would court big business to:
“work with the best of British business to reform the worst of British capitalism.”
Sebastian Whale (22 March 2020). “Wes Streeting: People in the Labour Party have got to start liking one another again”. The House.
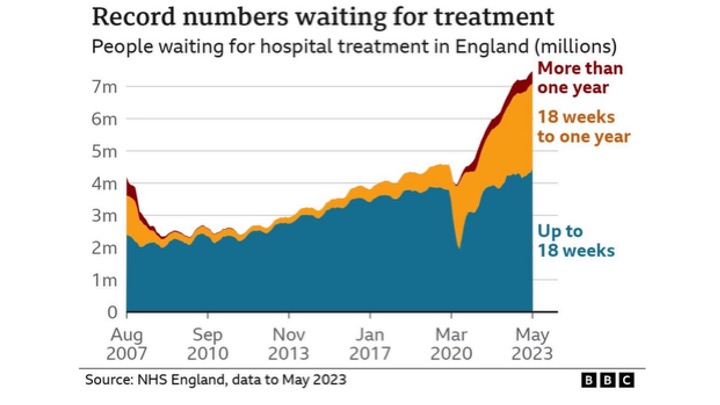
The Labour Party under Starmer is determined to “solve” the UK economic crisis by recourse to cutting the living standards of the working class. That includes complete stripping the NHS of its remaining prior state based funding. Private funding will substitute. . . with all that implies. The figure above of waiting lists for care – shows the direction the NHS is taking.
This article is from an NHS based consultant and health policy analyst, who exposes the Labour Party latest attacks on the NHS.
Editors, MLRG, 25 August 2025
Flawed assumptions, Alan Milburn and the ‘Ten Year Health Plan for England’
Alan Milburn was Secretary of State for Health from October 1999 to June 2003 before immersing himself in the world of private health care companies. He argues that the NHS can’t have more money than it has currently been allocated. Largely because this would take funding from other public services and from defence.
Repeating the mistakes of the past
Wes Streeting is the current Secretary of State for Health and Social Care since July 2024. Streeting credits Milburn as having delivered the shortest waiting times and highest patient satisfaction in the history of the NHS.
When first appointed Secretary of State for Health in 1999, Alan Milburn declared that the 1948 model of health care was not suited to today’s needs. He set about to entrench and institutionalise a market system within health care, advocating strongly for private finance deals. Now described as chief health advisor to the Minister for Health. He was appointed lead non-executive member on the Department Health and Social Security (DHSC) Board in November 2024.
Milburn has long argued to abolish NHS England. He is now keen to highlight failings in the NHS as an existential crisis, describing it as ‘a million times worse’ than when he was in office and very much ‘in the last chance saloon’.
A Labour spokesman commenting on Milburn’s recent return to the DHSC stated that:
‘Alan brings the insight and the knowledge of what made the biggest difference last time Labour was in office… It was the reforms on transparency, choice, and use of the private sector that delivered the goods on cutting waiting lists and making the NHS sustainable for the long term’.
Telegraph; but behind a paywall; But also see as cited in “Keep Our NHS Public” website article here
This view was strongly contested in an analysis by the 99% Organisation which argues cogently that increased investment was by far the most important element in improved NHS performance under New Labour, while various reforms had only marginal impact. This is a message the current government does not want to hear and studiously ignores. As with a planned return of private finance to build health infrastructure, there seems to be a dogged unwillingness to learn from mistakes of the past.
What have they prescribed for the NHS ? A “The Ten Year Health Plan (10YP)
The Ten Year Health Plan for England (10YP) states that technological developments will make the NHS more efficient and allow current resources to be used more effectively.
In terms of national resources, we are asked to accept that there is a ‘pie’ of limited size. This means that what is in fact an inadequate slice for the NHS should be regarded as generous given the prevailing economic conditions, while increasing the size of the slice would inevitably involve cuts elsewhere. The Treasury contends that to fund public services properly, we just need a bigger pie and this can only be achieved by economic growth.
“Hence, an effective health care system is not seen, as it was in 1948 when the NHS was born, as a necessary prerequisite for growth. Rather as something that must wait to be a beneficiary of future growth before it can materialise.
The 10YP considers that reforms are deliverable within the far from generous provisions of the recent spending review: ‘an extra £29 billion in investment will fund the reforms, service improvements and new technology required’.
Health Foundation podcast: Alan Milburn on the 10-Year Health Plan
It even sees prevention of illness rather than investment in staff and infrastructure as an answer to the negative effect on the economy of rising numbers of those unable to work through ill health. However these are token gestures.
Limited vision of the 10YP
This £29bn ‘record funding’ is actually less than the average historical annual rise in budget (needed to keep up with inflation and increasing demand). As Mathew Taylor, Chief Executive of the NHS Confederation pointed out:
‘this additional £29bn won’t be enough to cover the increasing cost of new treatments, with staff pay likely to account for a large proportion of it…..on its own, this won’t guarantee that waiting time targets are met.’
At HFMA.org.UK
The Nuffield Trust also commented that 2.8% is unlikely to be sufficient to enable the NHS to keep up with the routine increases in activity expected of it, let alone implement further government asks as in the TYP.
“Despite evidence showing that for every £1 spent on the NHS, £4 is generated for the economy, arbitrary fiscal rules act as a barrier to economic decisions that would actually improve people’s lives. Richard Murphy points out that the ‘Pie theory’ ignores the fact that when economic growth in past years has produced a larger pie, this has disproportionately benefited the rich, increasing rather than reducing inequalities.”
One Pound; and Nuffield
The crucial questions of ‘who is in charge of the oven?’ (e.g. the effects of government policies, corporate lobbying, etc) and issues of wealth redistribution are avoided. When US academics puzzled by Labour’s drive to partner the NHS with the private sector, they concluded this was ‘a covert means to redistribute wealth and income in favour of the affluent and powerful’.
Woefully inadequate assessment of costs and benefits in the TYP
a) Putative cheaper community care is a fallacy
The 10YP is full of techno-optimism but short on realism and lacks detailed analysis of costs and benefits. Many have challenged the assumptions on which it is based. For example, there is little evidence to suggest that good community care is really cheaper than hospital care. Thea Stein spent nearly a decade leading a community healthcare trust. She writes in the “Times” to strongly contest the view that moving care closer to home would save the NHS money. This is because community services identify unmet need which are expensive to remedy. Moreover hospitals benefit from economies of scale. Finally, she warned that:
‘if care is moved to a more efficient local or home-based setting, it can take many years to cash in any savings: closing wards or hospital beds cannot happen overnight’.
At Financial Times (behind paywall).
Worryingly also, we in the UK already have almost the lowest number of beds/1000 population among OECD countries.
b) Naivete of technological fixes on genetic screening
Sheldon and Wright expose how relying on newborn genome sequencing (genetic testing) to improve population health and reduce NHS demand – is a fallacy. They point to how easily politicians get seduced by technological fixes, and ask for the evidence that this will ‘transform the NHS over the coming decade, from a service which diagnoses and treats ill health to one that predicts and prevents it’. They ask too about the negative consequences and costs, emphasising:
‘it is the harms in particular that should concern us. Population genetic screening with its inherent false positives, false negatives, and unpredictable clinical consequences of mutations has the potential to generate a lifetime of anxiety for parents and their children. We run the risk of turning future generations into patients from the moment they are born, with over-diagnosis and over-treatment, as well as profound implications for how these data will be used by third parties such as life insurance companies’.
British Medical Journal
c) Wishful thinking on AI
Artificial Intelligence (AI) represents a multitude of evolving technologies. It is clearly not at this point a panacea for the ills of the NHS. Some even regard the claim that AI will transform NHS productivity as no more than snake oil, a false hope and potentially a bottomless money pit. Hope in AI is driven by marketing and not evidence. To imagine AI could transform the model of health care in the short term is highly unlikely.
Big tech (Microsoft, Google, AWS, Apple, Oracle) are already at the heart of the NHS. They remain crucial to the TYP. The negative consequences of the dominance of these companies (global theft of personal data and science knowledge from public institutions; harm to the environment and to human rights; direct destruction of human life through use by the military and for surveillance) are ignored. Far from aspiring to be a leader in technology, the UK government are all too happy to hand over data, infrastructure and public services to US tech giants, with an AI strategy based on techno-utopian assumptions.
What is the alternative?
Far better that politicians focus on tackling systemic societal inequalities that drive ill health and are amenable to government interventions. Labour’s 10YP has not thought these complex issues through. But they open up the possibility of profit driven companies enjoying a bonanza from marketing personal care in the form of targeted lifestyle, dietary advice and medication.
Milburn speaks to the Health Foundation
Milburn is the most prominent of many former advisors who assisted the notorious social democrat Tony Blair. Under Blair’s leadership, the Labour Party began the purge of traditional left trade unionists and workers influence, in favour of the bureaucracy representing business and finance gurus. His former advisors are now back in positions of influence.
Milburn’s recent interview with the Health Foundation makes the current direction of travel very clear. He argues that the centralised operating model for the NHS is wrong; that the NHS can’t have more money and that it is wrong to focus on acute care rather than prevention. His new ‘care model fundamentally should be about empowering the individual patient, citizen, to take greater control of their health’. He acknowledges that in the next three years Labour must deliver on GP and A&E access and waiting times. Over the following seven years there will then be long term change through use of genomics (genetic tests), digitalisation and workforce transformation.
Social determinants of health are dismissed as being outside the remit of the NHS:
‘the wider social determinants of ill health, poor housing, poor jobs, poor people, and all of that, and frankly, that broadly is outside the remit of the National Health Service’.
Meanwhile genetic testing is talked up as enabling a move from a ‘diagnosis and treat’ model to a ‘predict and prevent model’. According to Milburn, the combination of big data and genomic science will facilitate medical interventions both at individual and population health levels and be the focus of the neighbourhood health service. The danger of telling many individuals that they are ‘at risk’ and thereby fuelling demand for services is acknowledged. Apparently they wish to control this by applying financial flows to incentivise behaviour deemed appropriate by the centre. A key role here will be played by so-called “Integrated Health Organisations.”
Meanwhile, abolition of NHS England is consistent with the operating model government says it wants to see, which is ‘more delegated, more devolved and more diverse, and has to be smaller’. Milburn insists that we must stop seeing the health care system as being about a single institution (the NHS). Instead he argues it is an ecosystem involving telecommunication and technology companies, private sector providers and (lastly) the public sector. The job of the centre is to convene and manage that ecosystem.
“Change is not pain free. Nobody but nobody that I hear, anywhere across the system, is saying that it is currently sustainable.”
Milburn Podcast; Ibid at Health Foundation
Milburn is clearly listening to the wrong people. He should take heed of Lord Darzi’s review – ‘It is not a question of whether we can afford the NHS. Rather, we cannot afford not to have the NHS’. To put it another way ‘If the NHS is allowed to fail, the economy will fail with it – the UK economy cannot afford not to fund the NHS properly’. Darzi’s views that reform and further austerity were not the right prescription for an ailing NHS seem to have fallen on deaf ears.
An NHS consultant physician; August 25, 2025